Breathing a little easier
December 12, 2014
Share
Few of us would equate the household chore of vacuuming with quality of life. But for people with heart and lung disease, quality of life often comes down to having the breath, to carry out those simple, everyday tasks.
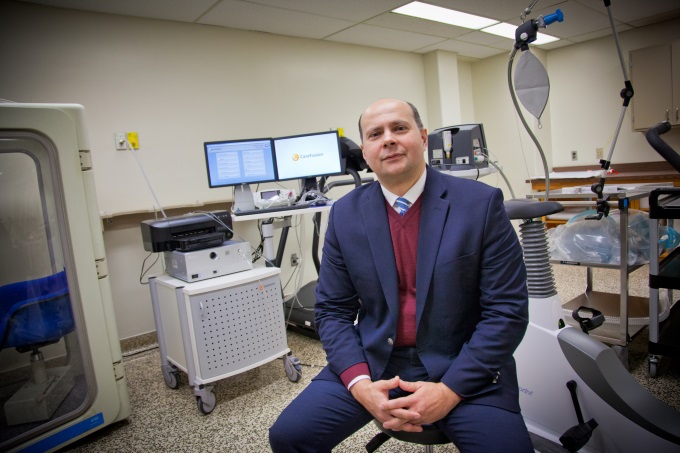
“There is a close relationship between your physical capacity and your quality of life,” says Alberto Neder, a Queen’s University respirologist and clinician scientist at the Kingston General Hospital Research Institute. “Shortness of breath has a huge impact on that quality of life.”
Born and educated in Brazil, Dr. Neder is a leading expert in exercise and respiratory physiology. He was recruited to Queen’s and the KGH Research Institute last year from the Federal University of Sao Paulo, where he was a full professor, head of the institution’s respiratory division, and founder of a rehabilitation centre for patients with chronic cardiac and lung disease.
Dr. Neder’s research focuses on the interactions of lungs, heart, blood and cells, with the goal of better understanding the mechanisms that cause the breathlessness associated with diseases such as Chronic Obstructive Pulmonary Disorder (COPD) and congestive heart failure. His long-term goal is to improve his patients’ quality of life.
“We are interrogating the complex biological system that is the human body. We’re not looking at just one specific system, we’re looking at all of them, and how they work in an integrated manner,” he says. “And the best way to investigate these systems is when they are under the stress of physical exercise. It gives us information we can’t get when the body is at rest.”
To do this he has established the Laboratory of Clinical Exercise Physiology at Kingston General Hospital, the world’s first centre devoted to the study of the combination of lung-heart disease. Patients take part in physical activities such as riding a stationary bicycle or walking on a treadmill, enabling Dr. Neder and his team to monitor and assess the complete oxygen pathway through the body, from oxygen intake and blood distribution to the work done by their respiratory muscles.
“By looking at all of these interactions we can discover what’s going on in terms of insufficient oxygen to the tissues, and how it’s linked to the sensation of shortness of breath and general fatigue.”
Dr. Neder’s research asks potentially game-changing questions about treatments for this difficult disease combination, and he is currently recruiting patients for at least three innovative studies.
One study assesses smokers with apparently normal lung function. The research aims to show, for the first time, early signs of COPD damage or malfunction to small lung vessels that are not apparent in conventional breathing tests. Currently little is known or done for those with COPD in its early, potentially reversible stages; this research could help to identify new treatments for early-stage COPD.
Another study, into congestive heart failure, explores the use of nitric oxide to improve blood flow to muscles including the heart and brain. Dr. Neder has begun the first randomized control study delivering concentrated beetroot juice, a natural nutrient that is rich in nitric oxide, to heart failure patients. “It has been used to enhance athletic performance, and now there’s the potential to use it as a health product,” he says.
“It’s about the benefits of keeping moving,” says Dr. Neder. “It makes a lot of difference, especially when you get older.”
This story is the fourth in a series on the KGH Research Institute, a collaboration between Queen’s and Kingston General Hospital, and the clinician-scientists recruited to work in the centre.